Upper Peninsula Health Plan ties for top-scoring Medicare-Medicaid Plan in nation

MARQUETTE — Upper Peninsula Health Plan (UPHP) tied for first place in the nation for overall rating of a Medicare-Medicaid Plan, according to a UPHP press release.
UPHP was approved by the State of Michigan and the Centers for Medicare and Medicaid Services (CMS) to provide the services of a dual eligible program called MI Health Link. The program is meant to make member’s Medicare and Michigan Medicaid benefits work better together. MI Health Link members use one plan and one card for health care, behavioral health care, home and community based services, nursing home care, and medications.
Under the Medicare-Medicaid Financial Alignment Initiative, the CMS measures the consumer experience through various methods, including beneficiary surveys. Under the capitated financial alignment model, Medicare-Medicaid Plans (MMPs) are required to annually conduct the Medicare Advantage Prescription Drug (MA-PD) CAHPS survey. The MA-PD CAHPS survey is designed to measure important aspects of an individual’s health care experience including the accessibility to and quality of services.
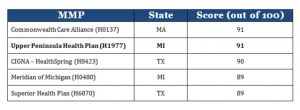
As part of the MA-PD CAHPS survey, respondents are asked to rate their health plan on a scale from 0 to 10, where 0 is the worst health plan possible and 10 is the best health plan possible. The scores below are the percentage of the best possible score each contract earned:
“We are thrilled that our members have positively rated our health plan to allow us this esteemed recognition. Managing the care for members who are dually enrolled in a Medicare-Medicaid Plan has its challenges. We do our best to keep our members satisfied with the services we provide, and it is wonderful to have their satisfaction reflected in the CAHPS score,” UPHP President and CEO, Dennis Smith, said in the statement.
In order to report MA-PD CAHPS in a given year, health plans, including MMPs, must have a minimum of 600 enrollees as of July 1st of the preceding calendar year. In early 2017, surveys were sent to a sample of MMP enrollees with at least six months of continuous enrollment. Enrollees were asked to evaluate their health care experience over the previous six months. As a result, 45 MMPs participating in nine capitated model demonstrations were able to report CAHPS during the 2017 reporting cycle.
Additional information regarding 2017 CAHPS results under the Medicare-Medicaid Financial Alignment Initiative should be available soon.
To learn more about UPHP, click HERE.
